Ebola Hematologic Disorders: Uganda Outbreak Highlights Gaps
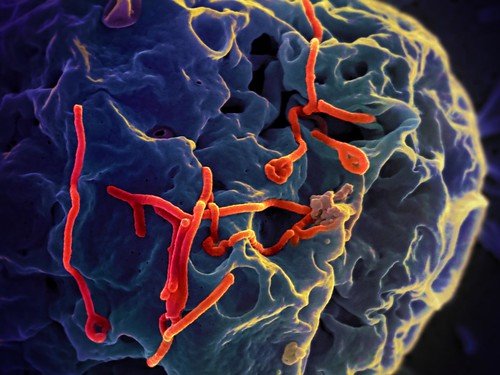
The 2025 Sudan virus (SUDV) outbreak in Uganda exposed critical vulnerabilities in global health security, highlighting the need for improved preparedness and response strategies. A new study published in *Zoonoses* reveals significant hematologic abnormalities in Ebola Virus Disease (EVD) patients, contributing to increased mortality. Simultaneously, the SUDV outbreak, unlike previous outbreaks, originated in the capital city of Kampala, rapidly spreading across multiple districts despite a robust response.
A retrospective study of 129 EVD patients hospitalized in Butembo and Katwa, Democratic Republic of Congo (DRC), from February 1, 2019, to June 25, 2020, found that hematologic abnormalities were prevalent. Anemia (55.8%) was significantly correlated with increased viral load and was identified as an independent risk factor for mortality (OR, 4.07; 95% CI, 1.59-11.3). Other abnormalities included hyperleukocytosis (36.4%), leukopenia (3.1%), thrombopenia (32.6%), and thrombocytosis (30.2%). Only 10% of patients had received the Ebola Zaire vaccine. These findings underscore the need for further research into the hematologic impact of EVD and the development of targeted treatments.
The Ugandan SUDV outbreak, led by National Incident Commander Dr. Henry Kyobe Bosa, presented unique challenges. The index case, a 34-year-old nurse, was diagnosed post-mortem, resulting in the rapid spread of the virus via two distinct transmission chains—an extended family and a hospital cluster—affecting three cities and over fifteen districts. This occurred concurrently with an ongoing mpox outbreak and amidst revised U.S. funding support for Ugandan health systems. Despite these challenges, Uganda launched a rapid response including the rVSV ring vaccination trial just four days after the outbreak declaration, deployed remdesivir from existing stockpiles saving 10 patients, and utilized cellphone data to track contacts.
Effective partner coordination, led by the Ugandan Ministry of Health (MoH) and the World Health Organization (WHO), was crucial. A national coordination committee was rapidly established, leading to timely interventions such as high-level meetings with local leaders and ongoing assessments of healthcare facilities. By March 31, 2025, 12 confirmed and 2 probable cases had been identified, with only two fatalities, showcasing the efficacy of the response. The outbreak highlights the importance of proactive surveillance, robust coordination amongst international and local partners, and the utilization of innovative tools in effectively managing future outbreaks. The ongoing need for sustained surveillance, community engagement, and strengthened global health security infrastructure remain paramount.